- Calls to this hotline are currently being directed to Within Health, Fay or Eating Disorder Solutions
- Representatives are standing by 24/7 to help answer your questions
- All calls are confidential and HIPAA compliant
- There is no obligation or cost to call
- Eating Disorder Hope does not receive any commissions or fees dependent upon which provider you select
- Additional treatment providers are located on our directory or samhsa.gov
What is Orthorexia: Symptoms, Complications and Causes
Orthorexia nervosa, while not an officially designated mental health diagnosis, is an increasingly concerning disorder. Evolving out of diet culture and the societal emphasis on “clean” and “healthy” food, orthorexic tendencies are viewed as socially acceptable due to a lack of understanding of the disorder and the dangers it presents.
Orthorexia Definition
The term orthorexia was coined in the 1990s by Steven Bratman, a practitioner of alternative medicine, and referred to “an almost pathological fixation on and obsession for healthy eating [1].” Individuals that struggle with orthorexia are typically focused on the quality as opposed to the quantity of food.
Orthorexia Nervosa DSM-5 Definition
It is important to clarify that Orthorexia Nervosa is not an official mental health diagnosis that is classified in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) or the International Classification of Disease (ICD-10).
Steven Bratman proposed possible criteria for Orthorexia Nervosa diagnosis in 2016 including:
- An obsessive focus on “healthy” eating and avoidance of “unhealthy” foods,
- Mental preoccupation regarding dietary practices, and
- Very rigid dietary rules with violations causing exaggerated emotional distress (fear of disease, anxiety, shame, and negative physical sensations) [1].
Many debate whether Orthorexia is a lifestyle phenomenon or a disease, however, “reports of physical (malnutrition and weight loss), psychological (fatigue and emotional instability), and social consequences (social isolation, diminished quality of life, and stigma) comply with current concepts of mental disorders [1].”
Even so, Orthorexia is more a term used to describe specific disordered eating tendencies and pathology but cannot be considered an independent mental disorder or official diagnosis.
Facts About Orthorexia
Despite the lack of diagnostic classification, orthorexia is still being widely studied and researched and the following statistics have been determined related to orthorexic prevalence:
- An estimated 21% to 57.6% of the general population engage in orthorexic behaviors [2].
- Rates of orthorexia may be twice as high in women as in men [2].
- Approximately 1% of college students struggle with orthorexic behaviors [3].
- An estimated 10% of the population is at risk for orthorexia development [3].

Signs of Orthorexia Nervosa
Orthorexia Nervosa behaviors can become severe diagnostic concerns and cause problematic long-term effects if not recognized and treated early. Below are warning signs that an individual’s eating behaviors may have become disordered.
Physical
Physical warning signs of orthorexic behaviors are more challenging to spot than other eating disorder diagnoses, however, there are a few indications [4]:
- Weight fluctuations.
- Reduced concentration.
- Difficulty sleeping.
- Vital/lab fluctuations.
- Constipation.
- Dehydration.
- Malnourishment symptoms due to food rules reducing the amount of food being consumed.
- Fine soft hair growth.
- Thinning hair due.
Behavioral/Emotional
Possible orthorexia nervosa behaviors can be more clear when considering the following behavioral and emotional symptoms:
- Obsession with the origin of foods (where/how prepared).
- Obsessive concerns regarding food and possible medical or health concerns.
- Rigid food rules.
- Increased supplement usage.
- Reduced consumption of food based on food rules centered on beliefs of “health.”
- Concern about food preparation and techniques and control over these things.
- Unwillingness to eat food not prepared by the individual themselves or whose preparation was not supervised by the individual.
- Judgment of those that do not adhere to their food rules.
- Linking self-esteem or self-view to adherence to food rules.
- Obsessively checking nutrition labels.
- Daily life revolves around food preparation or rules.
- Withdrawing from others.

Find a Treatment Provider
Dangers of Orthorexia
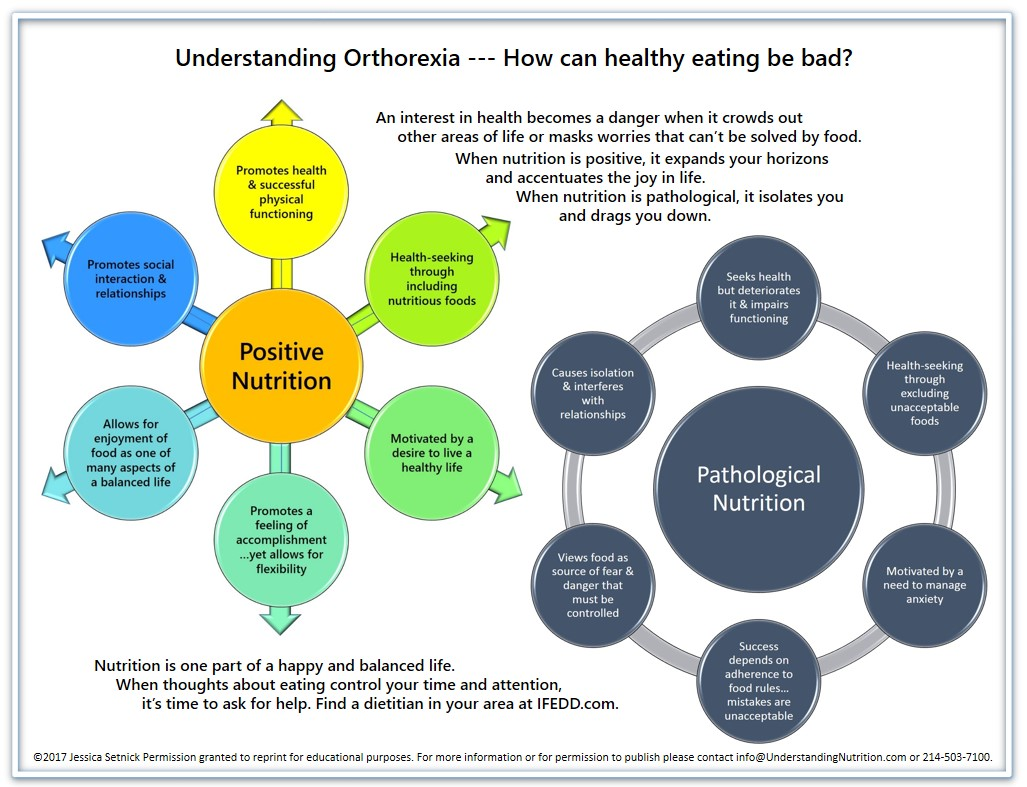
Many begin orthorexic behaviors to be more aware of what they are consuming and attempt to live “healthier” lives. Our societal beliefs and the impacts of diet culture and the wellness industry encourage many of the values held in Orthorexia Nervosa such as a focus on “purity” of food content and origin and “clean” eating. Emphasis on these aspects often becomes an obsession and results in food rules and rigidity that severely limit what an individual is comfortable consuming. Ultimately, what began as well-intentioned and socially accepted behaviors becomes disordered.
Long-Term Side Effects of Orthorexia Nervosa
Orthorexia Nervosa behaviors are often misperceived by society as “healthy” and “good” and, therefore, can go undetected or untreated. Without intervention, individuals become severely malnourished and can result in serious medical complications such as [5]:
- Malnourishment.
- Reduced cognitive functioning.
- Impaired immune system.
- Increased emotional dysregulation (IE: depression, anxiety, etc).
- Increased suicidal ideation and self-harming behaviors.
- Organ failure.
- Kidney issues.
- Alteration in menstrual cycle and function.
- Fertility issues.
- Cardiovascular and heart issues/heart disease.
- Isolation.
- Job performance impairment.
- Lowered bone density/osteoporosis
Click on Image to Enlarge
What Causes Orthorexia?
Like other eating disorders, there are various biological, psychological, and social aspects that contribute to development. Unlike other eating disorders, orthorexia can not only develop with approval from others based on social beliefs about food and the body, it can be perpetuated for the same reasons.
Biological Factors
Many of the biological factors that fuel anorexic beliefs and behaviors also fuel orthorexia, such as perfectionist tendencies. In other ways, orthorexia nervosa has similar neurological aspects to obsessive-compulsive disorder (OCD) such as obsessive fixations. Biological factors that contribute to orthorexia include:
- Family history of eating disorder behaviors.
- Perfectionistic and rigid personality traits.
- Obsessive personality traits.
- Childhood illness is related to diet or digestive issues.
- Medical problems that one believes can be cured through “pure” eating.
Psychological Factors
A large part of what contributes to orthorexia nervosa lies in psychology, as the disorder itself results from a cognitive fixation on the idea of “purity,” “cleanliness” and “health” in eating .Other psychological factors that contribute to orthorexia development include [6]:
- Low self-esteem/self-worth.
- History of past trauma.
- Co-occurring mental health diagnosis, particularly of OCD or Generalized Anxiety Disorder.
- History of dieting.
- Core beliefs are related to purity, cleanliness, and health as well as core beliefs related to food and self-worth, value, or morality.
- Disordered familial beliefs surrounding food “purity” and “health.”
- Tendency toward extremism and obsessiveness.
- Reportedly feeling pressure to be perfect or achieve perfection/success.
- Need for control.
Environmental Factors: Orthorexia & Social Media
As mentioned above, there is no doubt that, while society may not cause Orthorexic tendencies, the messages perpetuated about the body, food, and exercise via television and social media do not help. For example, one study learned that those following the “healthy eating” community on Instagram had a high prevalence of orthorexic tendencies [7]. Aspects of diet culture, the wellness and beauty industry, and social media that contribute to orthorexic beliefs are:
- Emphasis on eurocentric beauty standards and the “thin ideal.”
- Photoshopping and filters that alter the appearance without consumer’s awareness.
- Messaging that appearance is connected to empowerment/worth/fulfillment/etc.
- Lack of regulation around what is posted regarding laxatives/diuretics.
- Disguising laxatives and diuretics as lollipops and shakes that are “weight loss supplements.”
- Perpetuation of concepts that there are “quick fixes” to alter one’s body entirely from its biological predisposition.
- Lack of awareness of reality versus highly-curated social media.
- Reduced consumer consciousness.
- Increased feelings of unworthiness or lack of value or “measuring up” to false portrayals of life and “highlight reels” via social media.

How to Treat Orthorexia Nervosa
Treatment for orthorexia nervosa differs somewhat from the treatment of other eating disorders, namely because it is not yet a formal diagnosis. As such, those that struggle with Orthorexia Nervosa might be misdiagnosed with Anorexia Nervosa or diagnosed with Other Specified Feeding and Eating Disorder (OSFED) in order to receive insurance coverage for any treatment. While this does allow individuals to be treated, it often leads to miscommunication regarding their symptoms. Even so, the clinical community has not yet decided whether Orhotrexia is not a type of Anorexia Nervosa.
As researchers and treatment professionals figure this out, those struggling do not need to wait to receive support. The evidence-based treatment recommended for most eating disorders, such as Cognitive Behavioral Therapy (CBT), Family-Based Treatment, or Dialectical Behavior Therapy (DBT) is showing promise in also treating Orthorexia Nervosa [5].
If you or a loved one are currently struggling with the Orthorexic tendencies mentioned above, do not minimize or judge your struggles. Instead, acknowledge that you are feeling challenged and give yourself permission to care for yourself enough to seek help.
Speak With a Treatment Program
About Our Number
- Calls to this hotline are currently being directed to Within Health, Fay or Eating Disorder Solutions
- Representatives are standing by 24/7 to help answer your questions
- All calls are confidential and HIPAA compliant
- There is no obligation or cost to call
- Eating Disorder Hope does not receive any commissions or fees dependent upon which provider you select
- Additional treatment providers are located on our directory or samhsa.gov
Resources
- Strahler, J., et al. (2018). Orthorexia nervosa: a behavioral complex or a psychological condition. Journal of Behavioral Addictions, 7:4, 1143 – 1156.
- Ramacciotti, C.E., et al. (2011). Orthorexia Nervosa in the general population: a preliminary screening using a self-administered questionnaire (ORTO-15). Eating and Weight Disorders, 16.2.
- Dunn, T.M., et al. (2017). Prevalence of orthorexia is less than 1%: data from a US sample. Eating and Weight Disorders, 22:1.
- Scarff JR. Orthorexia Nervosa: An Obsession With Healthy Eating. Fed Pract. 2017 Jun;34(6):36-39. PMID: 30766283; PMCID: PMC6370446.
- Koven NS, Abry AW. The clinical basis of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015 Feb 18;11:385-94. doi: 10.2147/NDT.S61665. PMID: 25733839; PMCID: PMC4340368.
- Horovitz O, Argyrides M. Orthorexia and Orthorexia Nervosa: A Comprehensive Examination of Prevalence, Risk Factors, Diagnosis, and Treatment. Nutrients. 2023 Sep 3;15(17):3851. doi: 10.3390/nu15173851. PMID: 37686883; PMCID: PMC10490497.
- Turner, P.G., Lefevre, C. E. (2017). Instagram use is linked to increased symptoms of orthorexia nervosa. Eating and Weight Disorders, 22:2, 277-284.
Author
Publish Date:
Last Updated:
Page Last Reviewed and Updated By: Jacquelyn Ekern, MS, LPC on August 16, 2021